Imagine Sarah, a busy professional in her 50s, who feels generally healthy but hasn’t had a check-up in years. Her health plan reminds her to come in for an Annual Wellness Visit (AWV), where her provider identifies early signs of hypertension and prediabetes. Together, they create a proactive care plan that addresses these health concerns.
By identifying health risks and addressing them proactively, Annual Wellness Visits (AWVs) can help prevent the onset or progression of chronic conditions for patients like Sarah, reducing the need for costly treatments in the long run. Annual Wellness Visits (AWVs) also promote patient engagement by involving patients in their own care through education, goal-setting, and shared decision-making.
But it’s not just the patients who can benefit from Annual Wellness Visits (AWVs). Provider groups in risk-adjusted contracts and accountable care organizations (ACOs) can achieve more efficient resource allocation and improved financial performance through Annual Wellness Visits (AWVs). In fact, an NIH study found that Medicare beneficiaries who received an Annual Wellness Visit (AWV) experienced a 5.7% reduction in adjusted total healthcare costs over the next 11 months. Moreover, the patients who had an Annual Wellness Visit (AWV) were more likely to receive preventive clinical services.
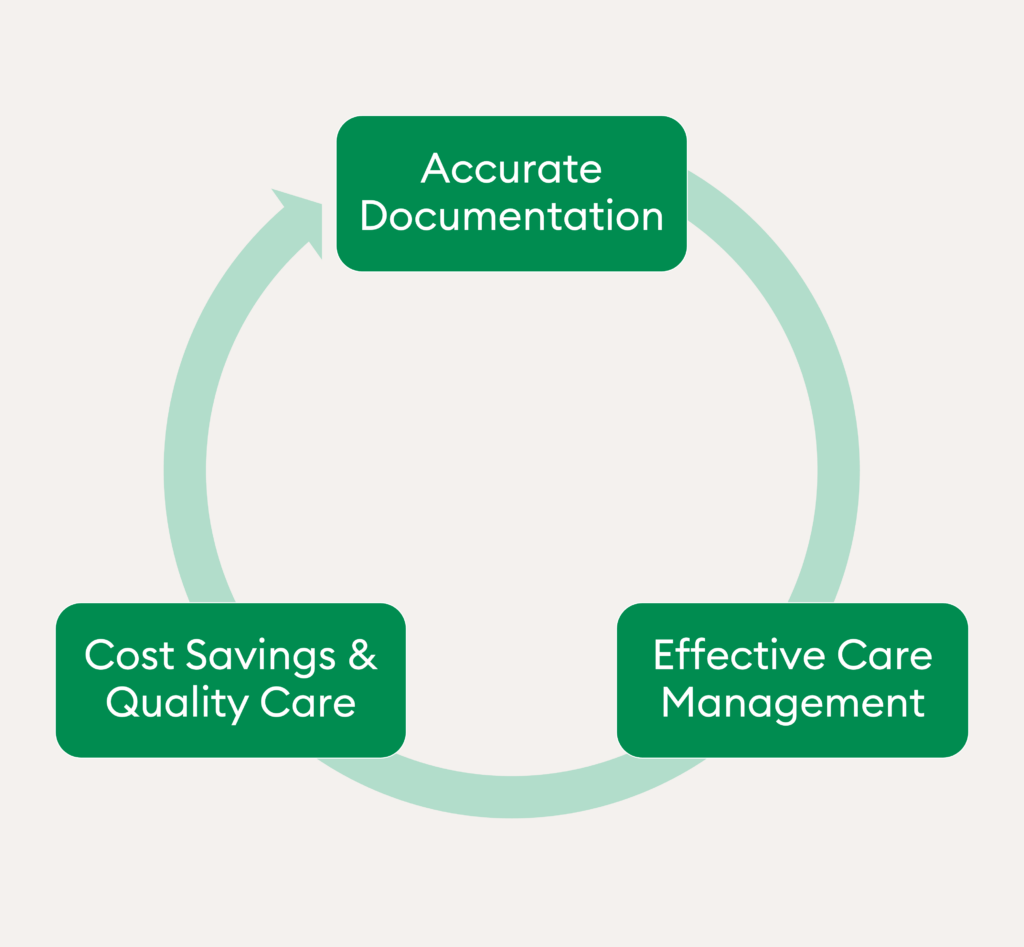
Thus, Annual Wellness Visits (AWVs) can help provider groups achieve value-based care’s goals of improving patient care while simultaneously reducing healthcare costs. So, what steps can you take to make your Annual Wellness Visit program more effective?
Step #1: Leverage Data to Identify Care Gaps
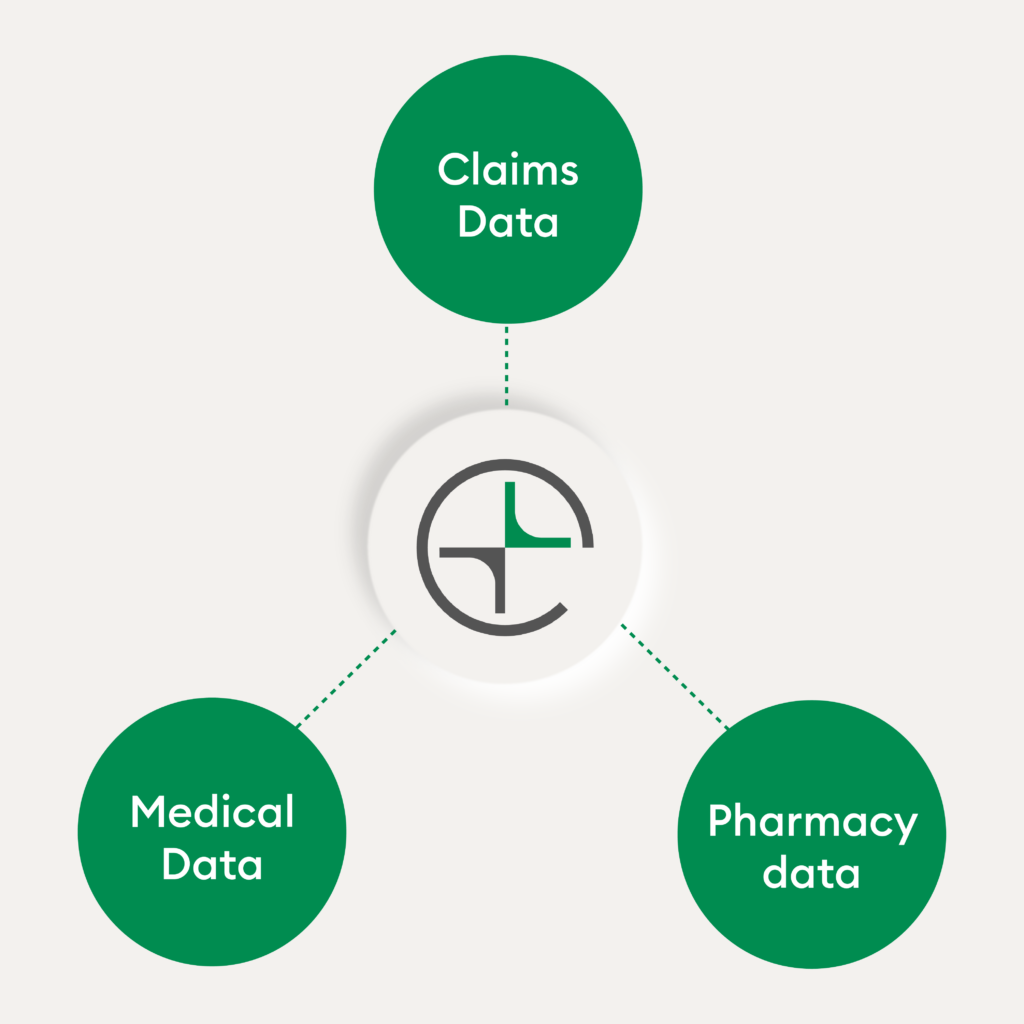
First and foremost, provider groups must have a holistic understanding of their patient population’s risk profile. For this, demographic information, medical history, and other risk factors should be pulled from multiple data sources, including the following:
After you gather a comprehensive set of patient data, you can then leverage analytics technology to accomplish the following:
- Identify missed preventative screenings
- Pinpoint gaps in data for specific member segments, such as for members new to the health plan or Medicare
- Surface potential chronic conditions that are not diagnosed or documented yet by using machine learning and natural language processing capabilities
An effective care gap identification tool should provide reliable evidence of any suspected conditions so that the provider can address them during the visit and close these care gaps.
Leveraging data effectively helps create and inform targeted interventions. This paves the way to high quality, patient-centered care while prioritizing care for the patients that need it the most.
Step #2: Enlist Risk Adjustment and Coding Support
Provider groups who lack in-house coding staff or resources can seek out support for documenting and coding AWV services. This can help alleviate administrative burdens and ensure accurate reimbursement for AWV-related services. Capturing this information accurately also helps clinicians create a comprehensive profile of the patient, which is important for designing the right care plan.
Beyond the individual patient, accurate coding also captures the complexity of the entire patient population served by the program. By accurately assessing patient risk profiles, including chronic conditions and comorbidities, healthcare providers can tailor preventative interventions and care plans to address individual needs effectively.
Provider organizations can take advantage of a pre-visit workflow tool to help prep their clinicians on the patients’ medical history before an AWV. This technology analytically distills the year-over-year diagnoses and clinically-suspected diagnoses that clinicians can address in advance of a visit, allowing for a thorough evaluation of patient health conditions. Since many AWV programs span the course of several months, any coding tool or service should be flexible enough to meet varying volumes and time frames.
Robust coding facilitates proper documentation and billing for AWV services rendered, leading to accurate reimbursement for the organization. Accurate coding also helps provider groups maintain compliance with regulatory requirements and minimizes the risk of audits or penalties associated with coding errors or improper documentation.
Step #3: Establish an Ongoing Reporting Process
After you finish building a strong AWV program, don’t rest on your laurels! Establish an ongoing reporting process that provides insights into program performance, patient outcomes, and healthcare costs. This enables healthcare organizations to identify areas of strengths and opportunities for improvements, guiding strategic decision-making and improved resource allocation.
Here are four key performance indicators (KPI) your provider organization can monitor to evaluate the success of your AWV program:
1. Number of completed wellness visits
2. Patient engagement levels
3. Number of gaps addressed and coded
4. Turnaround time for claims submission
You can also leverage these metrics to incentivize providers that achieve high patient engagement levels, total gaps addressed, or gaps closed around preventative care. On the opposite end, low-performing providers can be rolled into provider education series based on these insights.
From Reactive to Proactive: Annual Wellness Visits Key Role in Improving Value-Based Care Outcomes
In conclusion, AWVs are a vital tool for promoting preventative care and reducing healthcare costs. By identifying health risks early, patients like Sarah can develop proactive care plans that prevent chronic conditions from worsening. Provider groups and ACOs can also benefit from improved financial performance through effective AWV programs.
Key steps include leveraging data to identify care gaps, enlisting risk adjustment and coding support, and establishing ongoing reporting processes. By focusing on these three areas, healthcare organizations can enhance patient care, optimize resources, and achieve long-term financial sustainability.

