Over the past decade, the Centers for Medicare & Medicaid Services (CMS) has developed more than 50 Alternative Payment Models (APMs) with the goal of incentivizing low-cost, high-quality care for Medicare FFS beneficiaries. In April 2019, CMS announced the creation of the Direct Contracting Entity (DCE) model, which began its first performance year on April 1, 2021.
However, about a year later, CMS renamed the DCE to the ACO Realizing Equity, Access, and Community Health (ACO REACH) Model to place a greater emphasis on addressing health equity issues. Starting January 1, 2023, ACOs are participating in Performance Year 2023 of the ACO REACH model.
With REACH ACOs, CMS made one of its largest bets on value-based care to date, expanding participation to a wider group of providers than ever before. To help CMS accomplish its goal, ACO REACH organizations will need to maximize savings via targeted risk adjustment and patient engagement interventions — and this starts with beneficiary alignment.
Beneficiary Alignment Calculation
REACH ACOs are similar to other APMs in that their savings and losses are tied to the difference between annual expenditures of aligned beneficiaries and a financial benchmark calculated for those beneficiaries. Additionally, CMS currently plans to base their risk adjustment factor (RAF)calculations solely off of fee-for-service (FFS) claims data and Medicare Advantage (MA) Risk Adjustment Processing System (RAPS) data, without taking into account a separate stream of Hierarchical Condition Categories (HCCs) from chart reviews. This makes prospective risk adjustment and patient engagement interventions critical for DCEs.
To inform these interventions, REACH ACOs will need to anticipate who is aligned to their organization, how they are aligned, and if they are on track to align in the future. CMS calculates ACO REACH benchmarks by multiplying the number of beneficiaries by its base rate and risk score.

For each component of this calculation, there are associated questions REACH ACOs must be able to answer1:
- Number of Beneficiaries: In PY2, who will be aligned to my ACO REACH? Will they be voluntary or claims aligned?
- Base Rate: How will the base rate for those beneficiaries be defined?
- Risk Score: Based on my claims-aligned and voluntary-aligned beneficiaries, what will my PY 2022 risk score be?
CMS passively updates this calculation as claims flow in. Meanwhile, ACO REACH organizations can take additional steps to maximize savings by actively engaging with and optimizing each of these components, starting with understanding which beneficiaries will be aligned to their organization.
Who Will Align to Your ACO REACH and How
To determine which beneficiaries will be aligned, an ACO REACH should “clean” its pool of potential beneficiaries according to CMS’s alignment eligibility criteria, which differs based on the model:
Standard & New Entrant Eligibility Criteria2:
- Enrolled in Medicare Parts A and B
- Not enrolled in Medicare Advantage or any other Medicare managed care plan
- Not assigned, aligned, or attributed to another entity participating in a shared savings initiative
- Does not have Medicare as a secondary payer
- Resident of the U.S.
- Resides in a county that is included in the ACO REACH service area
Prospective Plus entering Q2, Q3, or Q4 Eligibility Criteria:
- Not aligned to another Medicare ACO REACH
Once an ACO REACH has determined which beneficiaries are eligible to align to its model, it must then consider how those beneficiaries may become aligned: through voluntary or claims-based alignment. For claims-based alignment, CMS will align an eligible beneficiary to a particular ACO REACH based on where they receive the plurality of their Primary Care Qualified Evaluation & Management (PQEM) services, as evidenced in claims utilization data. For a given payment year (PY), this algorithm takes data from the 24-month period spanning 30 months before PY start, to six months before PY start. This 24-month period is referred to as “alignment years.”
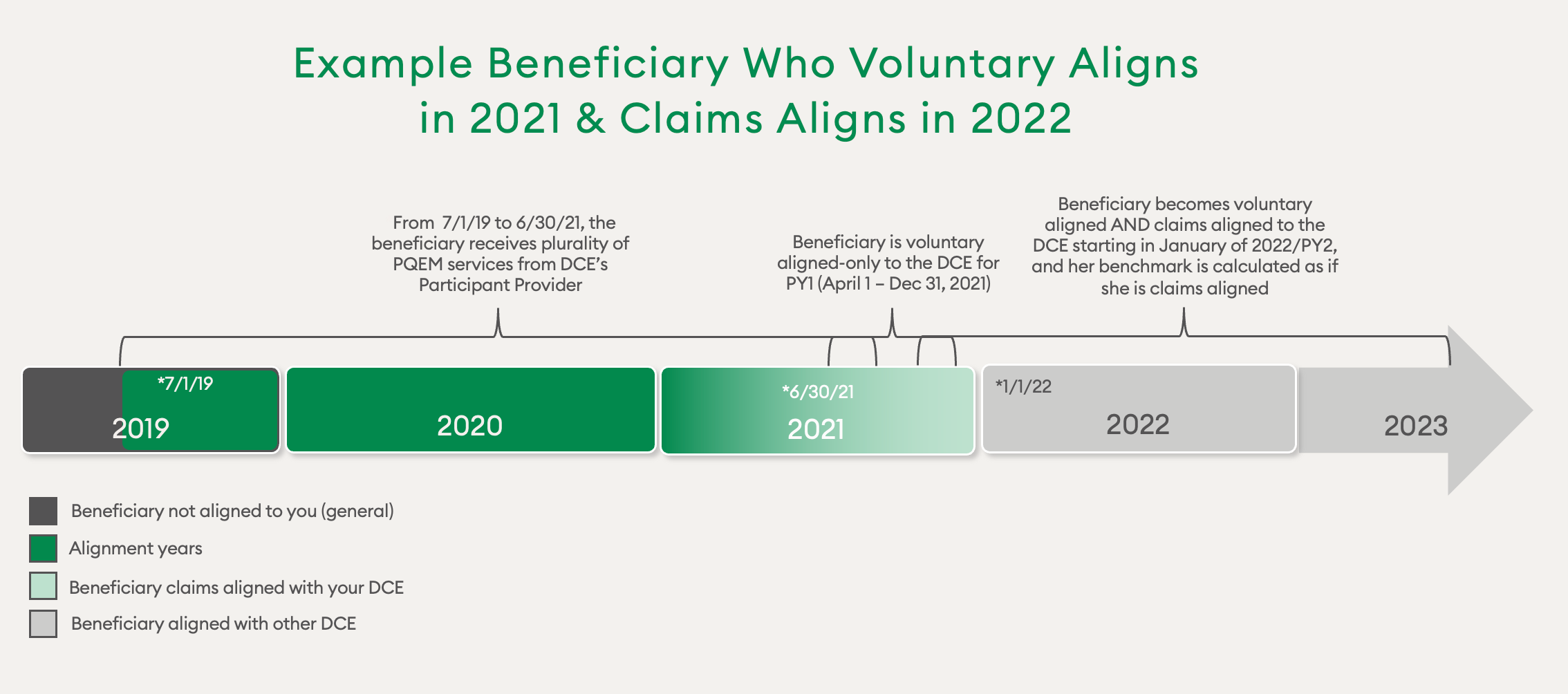
Beneficiaries can also designate a DC Participant Provider as their main provider and become voluntarily aligned with that provider’s ACO REACH the following PY. Under Prospective Plus alignment, this alignment comes into effect the following quarter. Voluntary alignment takes precedence over claims alignment. However, a beneficiary can be removed from voluntary-alignment if, in a PY, none of the ACO REACH’s Participant or Preferred Providers furnish services to the beneficiary and an outside provider submits a PQEM claim. While voluntary alignment comes down to a one-time human decision, claims-based alignment is based on an algorithm. This algorithm is straightforward and lends itself to REACH ACOs looking to track where their alignment is headed.
So, why does it matter how a beneficiary is aligned? Because the beneficiary base rate is based on whether they are claims aligned or voluntary aligned — and this can impact risk adjustment.
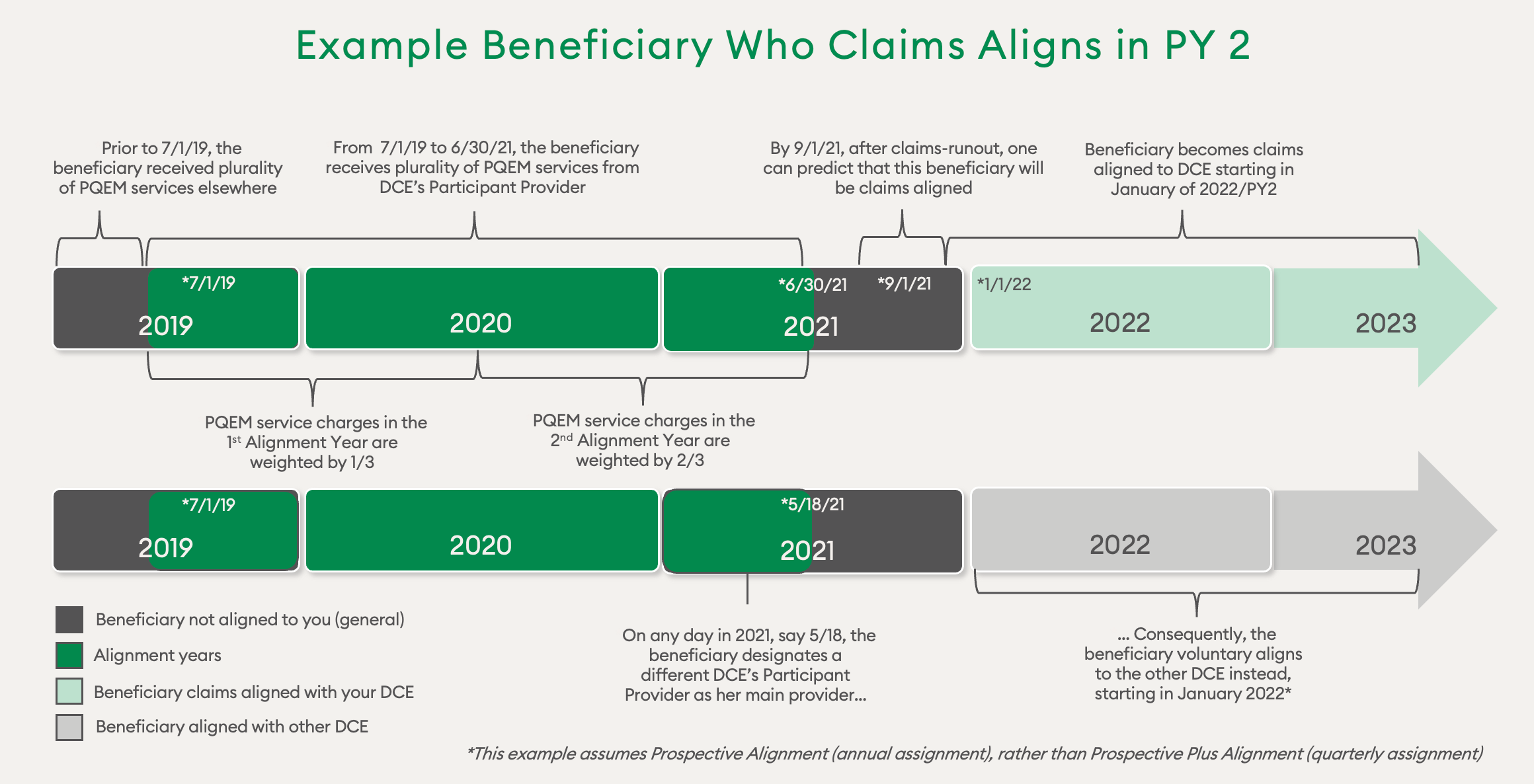
If a beneficiary meets the criteria described above, they can become both voluntary and claims aligned to the same ACO REACH. For example, a beneficiary who starts out with purely voluntary alignment to an ACO REACH will also become claims aligned once the plurality of their PQEM services in the alignment years are furnished by the ACO REACH.
How ACO REACH organizations conceive of this “both-aligned” beneficiary depends on the context of the question. For benchmarking purposes, this both-aligned beneficiary is treated as claims aligned. For questions about which organization they will align to in the future, their voluntary alignment status takes precedence over any updates to their claims-based alignment status.
How Beneficiary Base Rate is Determined
The way beneficiary base rate is defined differs based on whether they are claims aligned or voluntary aligned. For claims-based alignment, the base expenditure for beneficiaries for PY2 takes a blend of the PY regional rate (35%) and the 2017, 2018, and 2019 expenditures for beneficiaries who would have been aligned in those years, trended forward using the United States Per Capita Cost (65%).
The ACO REACH Regional Rate Baseline Adjustment converts the regional rate into this blended rate. For voluntary-alignment, the baseline is 100% based on the regional rate from the DC/KCC rate book, for the counties in which beneficiaries reside in PY22. In PY5, voluntary-aligned beneficiaries’ 2021, 2022, and 2023 expenditures are blended with the 2021, 2022, and 2023 regional rates to arrive at the benchmark. In PY6, the years 2022, 2023, and 2024 are used.
As mentioned above, the way a beneficiary is aligned impacts a ACO REACH’s risk adjustment. For claims-aligned beneficiaries, the PY 2/2022 risk score is capped at 103% of the 2020 reference year risk score (based on 2019 DOS).3 As an example, one might have a reference year risk score of 1.162. If the PY raw risk score is 1.200, it will need to be reduced down to 1.194 so as not to exceed 103% of the 1.162 reference year risk score.
For voluntary-aligned beneficiaries, the PY2 score is not capped at 103% of the 2020 reference year risk score, nor is it subjected to the Coding Intensity Factor. In this example, the PY2 raw risk score for voluntary-aligned beneficiaries is 1.24. Though this exceeds 103% of 1.159, this score is not capped. This exemption means that an ACO REACH has more freedom to adjust risk scores for voluntary-aligned beneficiaries.
Analytical Approaches to Alignment
Returning to the first question — who is aligned to my ACO REACH — it is worth noting that CMS will tell REACH ACOs in the form of de-identified alignment data as well as beneficiary-identifiable reports.
These reports include:
- List of DC beneficiaries
- Parts A, B, and D claims data, including Claim and Claim Line Feed (CCLF) reports
- DC Beneficiaries’ risk scores
- Monthly and quarterly reports of expenditures for Covered Services
- Quarterly financial reports for comparing PY Benchmark against expenditures
- Quality Performance Scoring Reports
CMS commits to providing information about a ACO REACH’s beneficiaries for a given PY in advance of that PY, but these reports are largely after-the-fact in scope and answer the question “Who has been aligned to me?” In order to execute impactful prospective interventions, an ACO REACH needs to ask this question well before it is finalized: “Who is on track to become aligned to me, or to align away from me?” An ACO REACH can extrapolate these counts going into 2022 by sorting their beneficiaries according to the rules of the claims-based alignment algorithm.
Case Study: Claims-Based Alignment Projection for 2022 & 2023
The table below considers beneficiaries currently aligned to a ACO REACH, and beneficiaries not-yet-aligned who may become claims-aligned to an ACO REACH. The negative numbers in parentheses represent those beneficiaries who are not aligned to the ACO REACH for the years in question (2021 vs. 2022 expectation). Beneficiaries who are “both-aligned” are made a subcategory of “voluntarily aligned” in the first table, but are subsumed within the claims-aligned in the bottom table for the purpose of benchmark calculation.
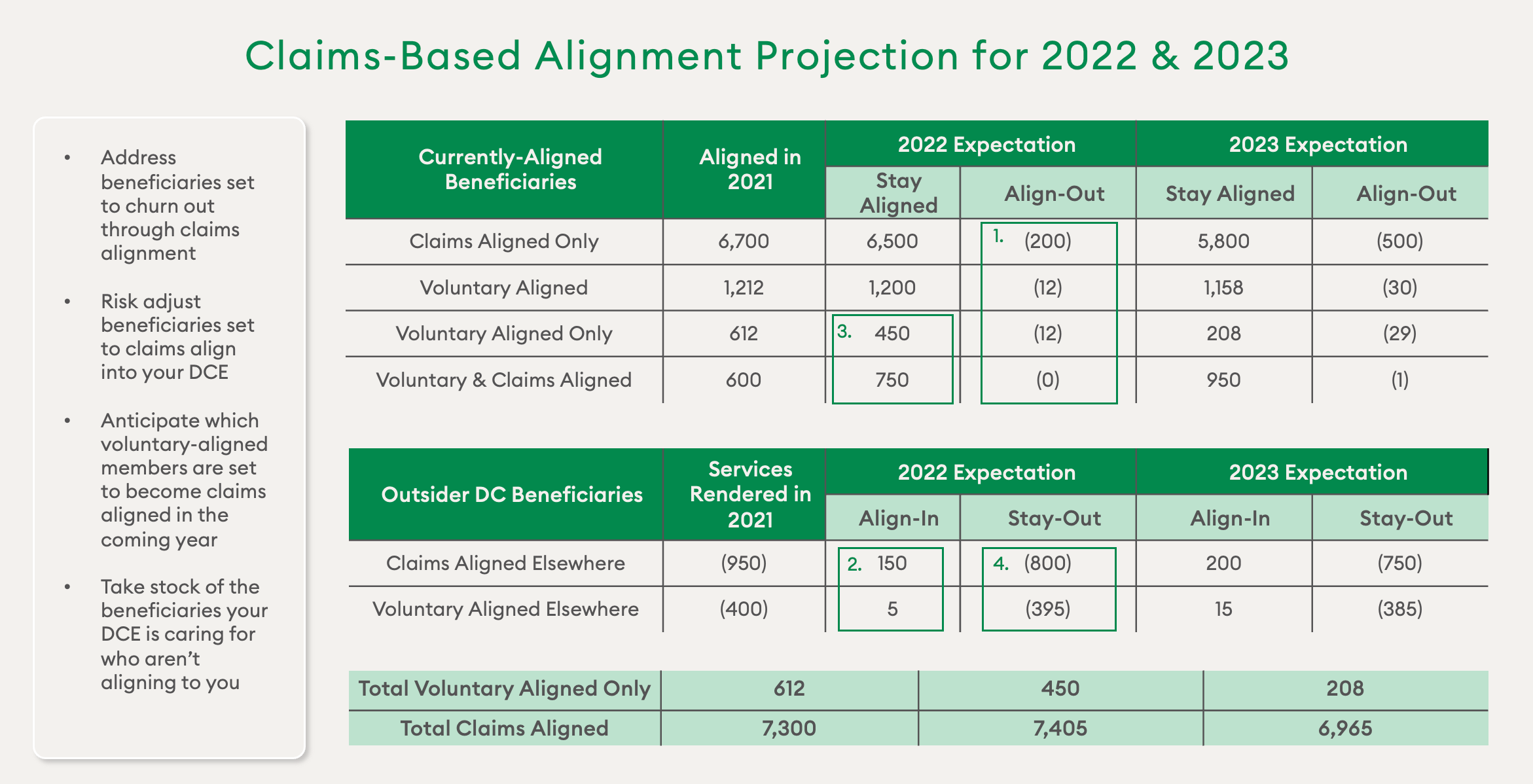
With these estimates, an ACO REACH may choose the following set of interventions for the distinct cohorts highlighted:
- Address beneficiaries set to churn out through claims-based alignment. Additionally, review which outside providers are submitting claims for them, as these could be candidates for contracting.
- Risk adjust beneficiaries set to claims align into the ACO REACH.
- Anticipate which voluntary-aligned beneficiaries are set to become claims aligned in the coming year.
- Take stock of the beneficiaries the ACO REACH is caring for who aren’t aligning to it
Any of these interventions can be further optimized by overlaying the level of need and cost for a given provider’s patients and prioritizing accordingly. A holistic estimate of enrollment for the coming year will allow an ACO REACH to check whether it risks falling below the minimum aligned beneficiary count. An ACO REACH may employ a combination of the interventions above to ensure this doesn’t happen.
Impacting the Benchmark
Since the benchmark is sized according to a ACO REACH’s risk scores, informed prospective risk adjustment interventions such as those described above will help ensure an accurate benchmark and increase an ACO REACH’s chances of enjoying savings.
An ACO REACH should target 6% RAF growth over the Reference Year for claims-aligned beneficiaries to ensure it hits the 3% cap on risk score growth. High-risk beneficiaries who are voluntary aligned (and thus exempt from the cap) should also be prioritized for risk adjustment. On the expenditure side, the same mapping can inform patient engagement and utilization management, enabling an ACO REACH to increase its savings in whichever benchmark it’s working with.
ACO REACH Toolkit for Beneficiary Alignment & Risk Adjustment
Once an ACO REACH understands the key principles of beneficiary alignment, they will need to develop a toolkit to put that information to use. The following capabilities are key for any ACO REACH looking to intervene systematically with its benchmark and expenditures:
- Data storage and tracking: Swift and comprehensive tracking of alignment-year claims to inform prospective intervention. Store data for easy access, search, and downloading in a secure fashion.
- Analytics and reporting: Project where beneficiaries are claims aligning (into vs. out of a ACO REACH). Predict instances of expiring voluntary alignment. Tier and prioritize beneficiaries according to level of need and cost. Project quality measure scores based on hospital admissions and other metrics
- Targeted risk adjustment interventions: Directed by analytics to ensure accurate and complete claims submissions.
While the ACO REACH model may add a layer of complexity to an organization’s financial operating plan, it represents an unprecedented opportunity for smaller provider groups to enter into the world of value-based care. ACO REACH organizations that are able to strategically leverage the model’s alignment algorithm and benchmark calculation will have a far greater likelihood of success than those that are reactive. Working with a strong risk adjustment analytics partner will be key to helping them break through the uncertainty, maximize savings, and ultimately help accomplish CMS’s goal of delivering low-cost, high-quality care.
For overburdened payers and providers, Episource helps close gaps in healthcare by marrying expert guidance with an end-to-end risk adjustment platform. Learn more about our solutions at Episource.com.
Footnotes:
1. The calculation also applies a discount, quality withhold, and retention withhold, which are not directly affected by alignment.
2. A third type, High Needs DCE, uses a set of alignment criteria which we are not yet covering for this blog post.
3. The CMS HCC prospective risk adjustment model uses a risk profile for a base year, e.g. 2019, to predict expenditures in the subsequent year, e.g. 2020.
This article was revised on 3.20.23 to replace all mentions of a Direct Contracting Entity (DCE) with CMS’s renamed model, ACO Realizing Equity, Access, and Community Health (REACH).

