In healthcare, understanding the Lifecycle of a Risk Score is crucial for accurately assessing and predicting patient risks, leading to effective care management and appropriate allocation of resources. Risk scores, also known as Risk Adjustment Factors (RAFs), play a significant role in this process. By quantifying an individual’s health status and associated costs, risk scores help healthcare organizations, insurers, and policymakers evaluate the potential financial risks associated with specific patient populations.
Components of a Risk Score
A risk score consists of two elements that together determine an individual’s expected healthcare costs. These elements include demographic factors as well as medical diagnoses. Demographic factors include age, sex, socioeconomic status, disability status, Medicaid eligibility, and institutional status (1). These factors, combined with medical diagnoses, provide a comprehensive picture of an individual’s overall health risk.
The Provider’s Role in Capturing Risk Scores
To ensure the accurate assessment of a patient’s risk score in the program, it is crucial for healthcare providers to submit all medical conditions that impact the patient’s health status. Since the risk score resets every January 1, failure to capture a chronic condition from a previous year will result in a decrease in the patient’s risk score for the current year. Conversely, if additional chronic conditions are reported, the patient’s risk score will increase compared to the previous year. (1)
The Relationship Between HCCs, International Classification of Diseases, ICD-10 Codes, and Risk Scores
Hierarchical Condition Categories (HCCs) are a key component of risk score calculations. These categories group similar medical conditions together, considering their severity and complexity. Each grouped HCC is assigned a factor that contributes to the overall risk score. In cases where multiple conditions within a category are present, the more severe or complicated conditions take precedence. This hierarchical structure ensures that the risk score reflects the true health risks and associated costs. (3)
ICD-10 codes provide a standardized system for classifying diagnoses. These codes are used to link specific medical conditions to the corresponding HCCs in the risk score calculation process. By assigning the appropriate ICD-10 codes, healthcare providers ensure accurate representation of a patient’s health status and enable an objective assessment of associated risks. (4)
How Risk Scores Are Calculated
The risk score for each individual is determined by considering their demographic details and medical diagnoses. The calculation of the risk score involves assigning weights to these factors based on their estimated impact on the overall risk. The final risk score is obtained by summing up the weighted contributions of these demographic and health care factors. Here’s an example:
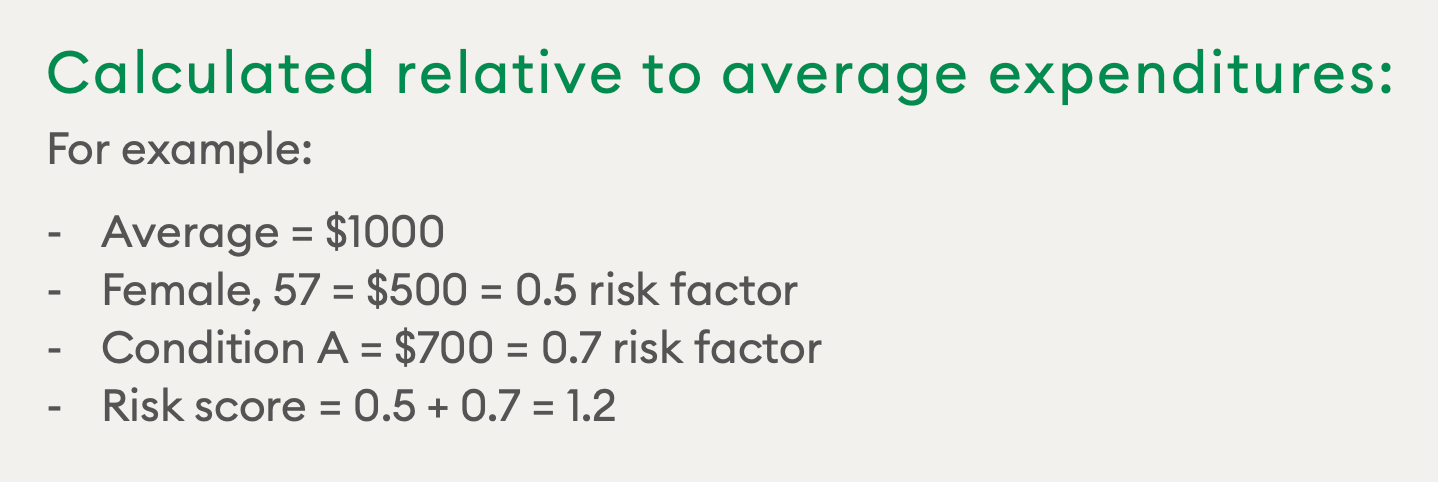
Source: CMS Presentation on Risk Adjustment Methodology
From Diagnosis to Risk Score
To illustrate how a risk score is determined, let’s say Greg is a 45-year-old male. Over the years, Greg was diagnosed by his physician with a number of conditions, which should be submitted annually.
1. Gather diagnosis and demographic factors: To assign a risk score to Greg, his diagnoses and demographic factors are collected. Risk scores are calculated based on a factor-based estimate of the expected costs or plan payment associated with Greg’s health conditions.
2. Grouping diagnoses into HCCs: Once the diagnoses, typically represented by ICD-10 codes, are collected and submitted, they are grouped into the appropriate HCCs. This grouping ensures that related conditions are considered collectively to provide an accurate representation of the individual’s health risk.
3. Documentation & ongoing management: Greg’s physician must properly document all relevant current and ongoing diagnoses that would affect his overall health.
4. Risk score calculation & variations over time: Then the risk score is calculated. Risk scores are not static, and are recalculated annually to reflect changes in an individual’s health status. Every year, Greg’s physician would have to capture all relevant diagnoses from the previous year as well.
Risk scores are essential tools for evaluating the health risks and associated costs within patient populations. By accurately assessing and predicting risk, healthcare organizations can enhance decision-making processes, optimize resource allocation, and deliver targeted interventions. Understanding the components and calculation methods of risk scores enables better collaboration among healthcare providers, insurers, and policymakers, ultimately leading to improved patient outcomes and more efficient healthcare systems.
Lear more, Risk Adjustment 101: Everything You Need To Know
References:
1. AAPC. (2023, May 2). What is risk adjustment?. AAPC. https://www.aapc.com/risk-adjustment/risk-adjustment.aspx#riskScoreRaf
2. Risk adjustment methodology overview – Centers for Medicare & Medicaid … (n.d.). https://www.cms.gov/CCIIO/Resources/Presentations/Downloads/hie-risk-adjustment-methodology.pdf
3. Hoffman, A. (2018, July). Average Beneficiary CMS Hierarchical Condition Category (HCC) Risk Scores for Rural and Urban Providers. NC Rural Health Research Program. https://www.shepscenter.unc.edu/wp-content/uploads/dlm_uploads/2018/07/Average-Beneficiary-CMS-Hierarchical-Condition-Category-HCC-Risk-Scores-for-Rural-and-Urban-Providers.pdf
4. Ameri Group – An Anthem Company . (n.d.). ICD-10-CM to CMS-HCC crosswalk – amerigroup provider sites. CMS-HCC Risk Adjustment Model (V24). https://provider.amerigroup.com/dam/publicdocuments/ALL_CARE_CMSHCCRAModel_mrdcoding_tips.pdf

