In 2010, the Affordable Care Act introduced various reforms to the healthcare system, including the creation of accountable care organizations (ACOs). ACOs aim to achieve the “Triple Aim” of improving health outcomes, enhancing patient experience, and reducing costs.
A mature ACO is a network of healthcare providers — including doctors, hospitals, and other healthcare professionals — who voluntarily come together to provide coordinated care to a specific group of patients (1). They are typically accountable for both the quality and cost of care provided to these beneficiaries. Presently, there are over 900 ACOs in the United States, operating in commercial, Medicare, and Medicaid markets, and serving more than 32 million individuals (2).
Types of ACOs
There are six different types of accountable care organizations that have been identified based on their organizational structure and the participants involved.
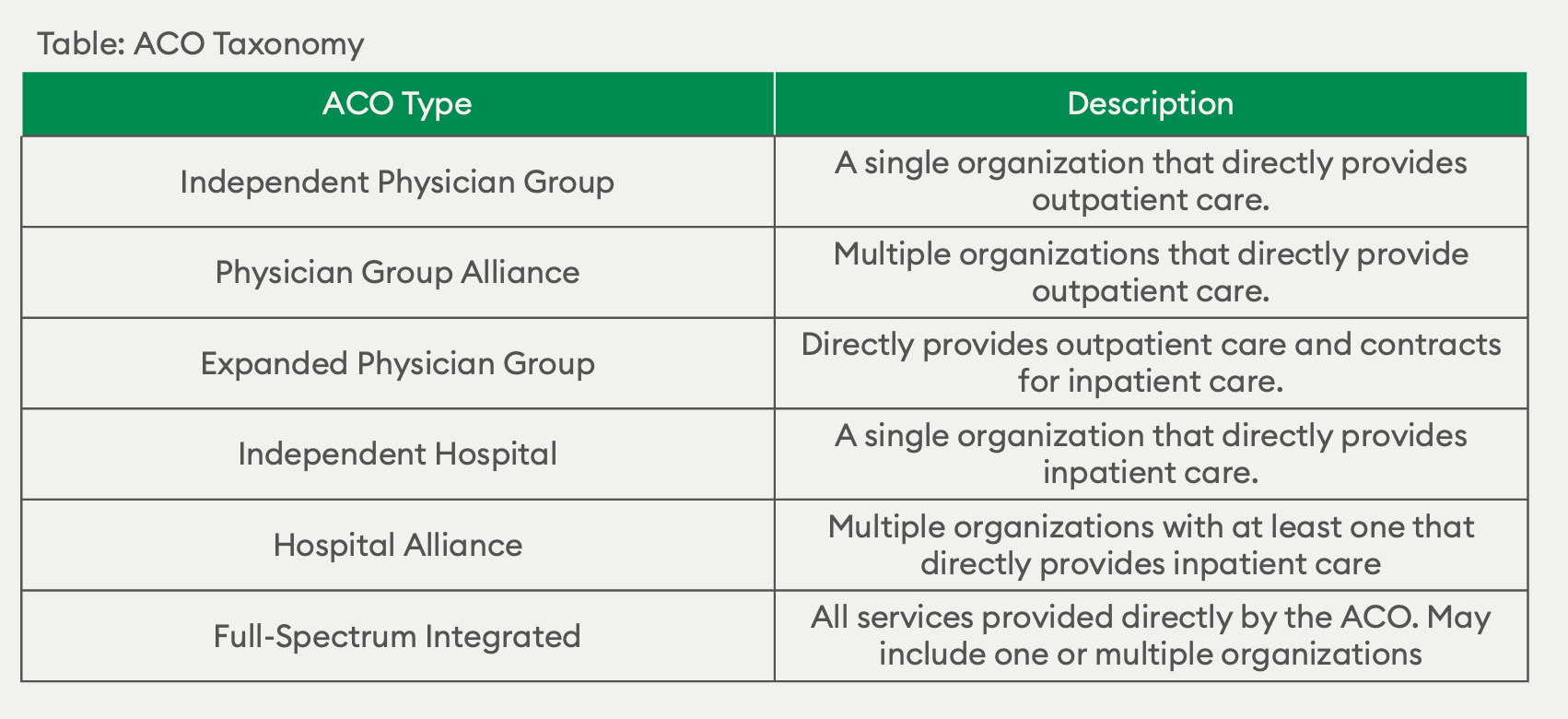
Source: Origins and Future of Accountable Care Organizations
Types of ACO Contracts
ACO contracts can vary depending on the type of organization involved and the payment arrangements in place. These contracts are often categorized based on the payer involved. The major participants in accountable care contracts include the Centers for Medicare & Medicaid Services (CMS), through programs like Pioneer, Medicare Shared Savings Program, and Advanced Payment ACOs. Additionally, there are Medicaid ACOs and commercial ACOs that engage with state Medicaid agencies and private insurers, respectively. (3)
Risk Scoring in the ACO REACH Model
Understanding risk scoring in the ACO REACH model is critical for success because it enables ACOs to effectively manage the health and financial risks associated with their patient populations. CareJourney’s article titled “Risk Scoring in ACO REACH Model” emphasizes the importance of risk scoring in optimizing ACO performance and achieving positive patient outcomes. (4)
The ACO REACH model focuses on identifying high-risk patients and providing them with targeted interventions to improve their health outcomes while reducing costs. Risk scoring plays a vital role in this process by assigning a risk score to each patient based on their individual characteristics, medical history, and predicted healthcare utilization. A strong comprehension of risk scoring will help ACOs in several key areas of operations and patient care:
- Targeted Interventions: A thorough understanding of risk scoring allows ACOs to identify patients who are at higher risk for adverse health events or costly healthcare utilization. This knowledge enables the ACO to prioritize resources and interventions for these individuals, thereby providing proactive and targeted care.
- Resource Allocation: ACOs can utilize risk scoring to allocate resources efficiently. By focusing on high-risk patients, ACOs can allocate resources such as care management, care coordination, and preventive services to those who will benefit the most. This strategic resource allocation improves the effectiveness of interventions and enhances patient outcomes.
- Financial Management: Accurate risk scoring helps ACOs assess the financial implications associated with managing different patient populations. It allows them to anticipate the expected costs of care, estimate potential savings, and negotiate contracts with payers more effectively. ACOs can also utilize risk scoring to identify opportunities for risk stratification and develop financial strategies accordingly.
- Performance Monitoring: Risk scoring provides a benchmark for evaluating ACO performance and progress over time. By comparing risk scores between different time periods, ACOs can assess the impact of interventions, track improvements in patient health, and identify areas for further optimization. This data-driven approach enhances accountability and facilitates evidence-based decision-making.
In conclusion, understanding risk scoring in the ACO REACH model is crucial for ACO success as it enables organizations to target interventions, allocate resources efficiently, manage financial risks, and monitor performance effectively. By leveraging risk scoring, ACOs can enhance patient outcomes, improve cost-efficiency, and drive the overall success of their accountable care initiatives.
References:
1. Accountable care organizations (acos): General information: CMS Innovation Center. Innovation Center. (n.d.). https://innovation.cms.gov/innovation-models/aco
2. Matulis, R., & Lloyd, J. (2018, February). The history, evolution, and future of Medicaid Accountable Care … – CHCS. https://www.chcs.org/media/ACO-Policy-Paper_022718.pdf
3. Tu, T. (2015, May). The impact of accountable care origins and future of … – brookings. https://www.brookings.edu/wp-content/uploads/2016/06/Impact-of-Accountable-CareOrigins-052015.pdf
4. Chaves, L. (2023, March 8). Why understanding risk scoring in ACO REACH is critical for Success. CareJourney. https://carejourney.com/risk-scoring-in-aco-reach-model/

